INTRODUCTION:
Several studies have disclosed the predictive role of tumor microenvironment (ME) in diffuse large B cell lymphoma (DLBCL). However, there is limited data regarding the prognostic impact of immune cells (IC) in the bone marrow (BM) of DLBCL patients (pts). Regulatory molecules secreted from primary tumor sites may induce a pro-tumorigenic ME within BM, resulting in an impaired systemic immune response that could promote lymphoma survival.
AIMS:
-To determine the prognostic impact on survival and risk of early relapse (ER) of the % of T lymphocytes (TL), monocytes (Mo), neutrophils, NK cells and polyclonal B lymphocytes (BL) measured by flow cytometry (FC) in pre-treatment BM aspirates of DLBCL pts.
METHODS:
We selected pts with DLBCL and available BM aspiration FC data at the time of diagnosis who received treatment at our institution between 2012 and 2019. Clinical information was collected from medical records.
FC analysis was performed with 8-color FC panels according to international Euroflow protocols. % of TL, Mo, neutrophils, NK cells and polyclonal BL by FC were compared to the normal values determined by Matarraz et al. (Cytometry part B, 2010). All parameters were analyzed as ordinal variables in 3 categories: low, normal and high.
Odds ratio for ER (relapse within a year) was calculated using logistic regression. The survival analysis was estimated with Kaplan-Meier method. The comparison between variables was performed through log-rank test and multivariate analysis with Cox regression.
RESULTS:
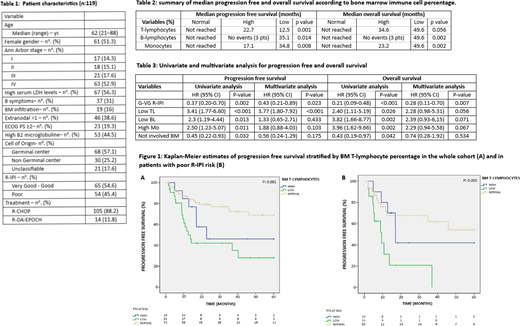
A total of 119 pts were included in this retrospective study. Pts characteristics are summarized in Table 1. All pts were treated with immunochemotherapy regimens. Median PFS and OS were not reached, 75th percentile of 12.7 and 27.8 months (m), respectively; with a median follow up time of 30.7 m (range: 3.4-60). ER was documented in 25 pts.
Regarding BM IC, pts with normal TL, polyclonal BL and Mo % were significantly associated with superior PFS and OS (figure 1A and table 2). No correlation between BM NK cells or neutrophils levels and outcome was observed. Moreover, BM IC levels did not statistically differ in involved vs not involved BM.
In our cohort, the R-IPI was able to discriminate outcomes in poor and good-very good (G-VG) risk (median OS of 48 m vs. not reached, p <0.001; and median PFS of 34.8 m vs. not reached, p: 0.001, respectively). Histopathologic involved BM also predicted inferior survival (median OS of 48.3 vs not reached, p:0.037; and median PFS of 16.9 m vs not reached, p:0.028).
R-IPI, BM involvement and BM IC were included in a multivariate analysis. G-VG R-IPI and low BM TL % remained independent prognostic factor of PFS on multivariate analysis with HR of 0.43 (95% CI 0.21-0.89, p: 0.023), and 3.77 (95% CI 1.8-7.92, p <0.001) respectively (Table 3).
The odds of ER was 4 times higher in pts with low BM TL % (95% CI 1.47-10.84, p: 0.006) and 2.8 times higher in pts with low polyclonal BL (95% CI 1.07-7.58, p: 0.036). On the contrary, G-VG R-IPI showed a protective effect with an odds ratio for ER of 0.22 (95% CI 0.08-0.61, p: 0.003). On multivariate analysis both the low BM TL % [OR 5.18 (95% CI 1.45-18.53, p: 0.011)] and the R-IPI subgroup [OR 0.21 in G-VG R-IPI (95% CI 0.06-0.71, p: 0.012)] were predictive of ER.
Pts with poor R-IPI were subsequently stratified according to BM TL categories. Pts with low and high TL % had a median PFS of only 9.4 vs 17 m respectively. However, it was unexpectedly not reached in the normal TL subgroup, p: 0.005 (Figure 1B). There was also a trend towards inferior OS in pts with low and high TL (median of 23.1 and 27.8 m respectively vs not reached for the normal subgroup, p: 0.09).
CONCLUSIONS:
Normal BM % of TL, BL and Mo in DLBCL pts measured by FC was associated with better outcomes in our cohort irrespective of BM involvement. Furthermore, concomitant low BM TL% and poor R-IPI identified a subgroup of pts with extremely poor results. These two variables presented at diagnosis might be used as prognostic factors of early relapse in DLBCL. In the future, therapies that could target the crosstalk between lymphoma cells and the BM ME might represent an encouraging strategy to improve outcomes in DLBCL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.